In her mid 20s, Chandell was diagnosed with a lung disease that causes inflammation and scarring (fibrosis) of the lungs. Prior to the diagnosis, Chandell attended college and was successful in her career as a Production Lead for Schweitzer Engineering…
Sandee Rudy’s enthusiasm and zest for life is evident as she describes her and husband Scott’s shared passion for cycling. Last year alone, Sandee logged an impressive 3,000 miles on her bike.
Most of us don’t think twice about the ability to breathe. But the simple act of inhaling and exhaling on his own is something Francisco “Pancho” Ibarra will never take for granted again.
It wasn’t always that way, though. Pancho had never even contemplated the inability to breathe. Pancho, 53, runs a thriving business, Pancho’s Heating and Cooling in the Tri-Cities. The self-proclaimed workaholic worked full-time and spent his weekends helping family and friends with their projects.
Everything changed when Pancho contracted COVID-19.
Read moreWilliam “Bill” Stryker is no stranger to breathing problems. Bill lives with chronic obstructive pulmonary disease (COPD) and requires two to four liters of oxygen supplementation 24 hours per day. He is also a survivor of tonsillar cancer, though the chemotherapy and radiation treatments left him with a feeding tube and loss of taste.
Despite his medical history, Bill remained an active 76-year-old. For many years he lived in Sacramento, California, operating a business. Now living in Deer Lodge, Montana, Bill remains active with daily chores, including shopping, cooking, and cleaning, as well as tinkering around his garage.
The day after Thanksgiving, things changed quickly. Bill didn’t feel well and required much more effort to breathe. His local hospital assessed him before quickly transporting him by air to St. Patrick’s Providence Hospital in Missoula, Montana.
Bill was diagnosed with acute hypoxic respiratory failure due to COVID-19 pneumonia. He also suffered from a left-sided pneumothorax, commonly known as a collapsed lung. His body required very high oxygen supplement.
For the next 37 days, Bill fought for his life at St. Pat’s.
On three separate occasions, three different doctors discussed hospice care with Bill. He wasn’t sure he was going to be able to beat this. But Bill prevailed and his health began to stabilize.
On January 13th, Bill was finally stable enough to tolerate the three-hour ambulance transfer to Northern Idaho Advanced Care Hospital (NIACH). Located in Post Falls, Idaho, NIACH is the only long-term acute care hospital within 300 miles. It is also the only long-term acute care hospital in Idaho certified by The Joint Commission for respiratory failure.
Each day, the pulmonary intensivist and multidisciplinary team at NIACH worked with Bill to improve his lung function and oxygen saturation during movement with therapies. Bill was a very motivated patient. “A body at rest, rots,” was his mantra during his stay. The NIACH staff found his motivation contagious.
After several weeks, Bill discharged to his home in Deer Lodge on his usual two-to-four liters of oxygen. His son and daughter-in-law picked him up, and he walked down the 150-foot hallway at NIACH without the use of an assistive device.
“This hospital is a very nice place,” Bill said before leaving. “I will tell everybody about it. Your physicians, respiratory therapists, nurses, and therapists are very knowledgeable about treating pulmonary issues. They encouraged me to use the incentive spirometer and to keep moving. I even got my feeding tube out from my previous cancer issues while I was here!”

In need of a hospital specializing in medically-complex patients, Calvin Dustybull came to Northern Idaho Advanced Care Hospital
After undergoing heart surgery, Calvin Dustybull had a complicated recovery. Calvin has a complex medical history, including coronary artery disease, mitral stenosis, chronic atrial fibrillation, and diabetes with advanced chronic kidney disease. The 62-year-old faced a long and complicated recovery before he could safely return home to his two sons in Browning, MT.
Twenty days after a quadruple coronary artery bypass grafting, Calvin still needed a high level of medical care. He required a ventilator, dialysis, and an NG tube for feeding. He also suffered from encephalopathy (altered mental state) and thrombocytopenia (low blood platelet count). For self-care activities, Calvin required the assistance of others.
Calvin needed a hospital that specialized in managing medically-complex patients like himself. His care team at Benefits Hospital in Great Falls, Montana referred him to Northern Idaho Advanced Care Hospital (NIACH).
At NIACH, Calvin began to make progress in his recovery. The pulmonary intensivist team and clinicians weaned him off the ventilator. Soon, he was decannulated and breathing room air. Over the course of five weeks, Calvin received dialysis three times per week. With nutritional support and therapies, his strength improved. Except for a slight memory deficit, Calvin’s encephalopathy resolved, as well.
Calvin recalls the staff at NIACH encouraging him to work hard and keep fighting each day. “At the beginning, I couldn’t speak or remember my name,” Calvin said of his admission to NIACH. “But with the help of therapies and encouragement from the staff, I remained focused on my goals and my memory started to improve.”
With a strong foundation to build on, Calvin was ready for the next stage of his recovery. However, his needs remained great. Calvin’s care plan required continued hemodialysis, therapy for strengthening, wound and stoma care, anticoagulation management, diabetic management, and continued nutritional support. This led Calvin to Rehabilitation Hospital of the Northwest (RHN). RHN shares a campus with NIACH in Post Falls. There, Calvin would receive the medical care he needed while receiving more intensive therapy. For three hours each day, Calvin received physical, occupational, and speech therapy at RHN.
Throughout his stay at RHN, Calvin made great strides in his recovery. He increased his independence with transfers and activities of daily living. His mobility improved to ambulating 120 feet with a four-wheel walker. Speech therapy helped address his mild cognitive defects. Calvin also made progress with his diabetes. He no longer required insulin, with his hemoglobin A1C down to 5.8.
Calvin attributes his great outcomes to goal setting and the team approach at both NIACH and RHN. He expressed appreciation for the education he received, as well. The staff taught Calvin about his medical conditions, medications, exercises, and assistive devices. They also shared ways to increase his safety, strength, and function at home. This education carried over to his loved ones, as well. On Calvin’s discharge day, his two sons and a friend participated in caregiver training. Staff informed them of necessary follow-up appointments they had set for Calvin, too.
Calvin and his loved ones were excited for his return home. They planned a cookout with his grandkids and friends to celebrate his success. Calvin continues to gain additional strength each day, utilizing the education he received at NIACH and RHN.
It was a journey that would forever change their lives.
At 4:00 a.m, Barb Hollace took one look at her husband and said, “You’re not OK.” Her husband, 74-year-old Bill Hollace, had been coughing for a couple of days and was not looking good that morning. Barb called an ambulance. Bill was taken to Valley Hospital in Spokane Valley, WA where he was diagnosed with pneumonia. That night, the hospital staff informed Bill that they thought he was having a heart attack, despite the fact that he wasn’t feeling any symptoms. Three days later, while still at Valley Hospital, he was diagnosed with Influenza A. The following morning he had a stroke.
Bill was immediately transferred to Deaconess Medical Center where he underwent surgery. Deaconess and Valley Hospital are both a part of the MultiCare Hospital system. All strokes within the MultiCare system are transferred to Deaconess, which is the only Spokane hospital to have earned the Joint Commission Stroke Certification.
Bill spent the next 50 days at Deaconess in the intensive care unit as he recovered from his multiple health issues. About two weeks into his stay, he was placed on a ventilator due to respiratory failure. The Hollaces received what they described as great care from a dedicated staff.
During Bill’s stay in ICU, there were a lot of conversations about next steps, such as discharging to a skilled nursing facility who could manage a ventilator. But after ongoing conversations between Barb and several ICU nurses, it was suggested that Bill needed to transfer to North Idaho Advanced Care Hospital (NIACH) in Post Falls, Idaho. Although this would mean moving Bill out of their home state, in Barb’s mind, her greater concern was Bill’s care.
Dr. Coulston, Medical Director, Intensive Care Unit at Deaconess also recommended NIACH because of its reputation and high standards. Barb trusted Dr. Coulston with Bill’s life and highly valued his opinion. Ultimately, after looking at the NIACH website and reviewing testimonials, Barb chose to continue Bill’s journey at NIACH. Barb said, “We had to finish his journey well. Nothing less than top-rate care was acceptable. We needed to give Bill the best chance at life.”
Great care is what they got at NIACH, according to Barb. “The very first day that we were at NIACH, we were getting work done,” said Barb. “The trach was downsized; we were working on mobility.”
Barb also commented that “the respiratory therapists at NIACH have the system down. They know when to push. Not too far, but still stretching the envelope. NIACH provided an amazing opportunity for him to get weaned off the ventilator, and step by step getting closer and closer to his recovery.” The Hollaces also found that the medical providers went above and beyond by working consistently through the Easter weekend to secure a pacemaker placement for Bill. The pacemaker was a huge step forward in Bill’s recovery process.
Una Alderman, CEO of NIACH, would wave at Barb when she saw her arrive. “Una made it personal. Everyone there did, from housekeepers to the front desk, we had the best. We received so much encouragement and affirmation along the path.” Bill added, “They made me feel like I could beat this. They were the support right there to encourage and push.”
Barb recalled hearing someone say, “Miracles happen here, all the time.” Bill was named the “Miracle Man” at Deaconess because of his amazing recovery. Barb knew they were in the right place at NIACH.
From the very beginning of this journey, Barb’s belief was that Bill would walk again. At first, Bill wasn’t able to participate as much as he would have liked to with physical therapy, due to the magnitude of his medical issues at the time. The Hollaces, though, were hopeful that Bill would soon be able to participate with therapy in such a way that he could transfer to the Rehabilitation Hospital of the Northwest (RHN). RHN is the sister facility to NIACH and sits on the same campus.
To accomplish this, the Hollaces, when medically ready, chose to continue their “Road to Rehab” at Life Care Center in Post Falls (a skilled nursing facility) in hopes of increasing his strength and endurance for admission to RHN. Bill hit a bump in the road during his two weeks at Life Care with a reoccurrence of his pneumonia. “We took a little detour and got to come back to NIACH a second time,” Barb said, “which on one hand was a bummer, but on the other hand, how cool is that! Bill was able to start eating and advancing his diet during that second time, and he was able to do more physical therapy. Then, we got to go to RHN to “polish the diamond” is what I liked to call it.”
According to Barb, coming to RHN was a different experience. “Three hours a day of therapy…kind of like boot camp, huh, Mr. Bill?” she chuckled to her husband. “Coming to RHN was a blessing; they encouraged family members to be there. We learned so much from family involvement and training.” Family members are encouraged to stay there, which Bill found as a great opportunity “to see if we were still compatible.”
Bill remembers the daily, jovial jousting between himself and the RHN therapists. He would say, “Let’s challenge me.” And they would. Bill wanted to be challenged as he didn’t want to get bored. Bill talked about how the therapists at RHN didn’t make him feel like he was part of the masses or only a number. They were there for him and his individualized care. Bill said, “They made fun out of it and that helped the stress back away.”
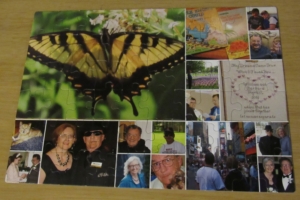
Barb made this puzzle, filled with memories of their past, to help Bill with his memory during recovery. The butterfly represents the transformation that has occurred and hope for the future.
There were tough moments, too. Barb called them the “breakthrough parts.” There was a “blow up” when he was working with the speech therapist on math, using coins. Bill said, “I need to have a way to measure my progress.” They started recording his progress on a chart on the bathroom door. It was very beneficial for Bill to see his progress. It helped him to understand why he was there and doing what he was doing. Bill felt as though he was a part of the team instead of only doing things that he was told to do.
In preparation for Bill’s discharge to home, Erik, a physical therapist at RHN, went to Bill and Barb’s home to do a home evaluation to see what obstacles Bill might encounter when he returned home with his wife. They realized that going up eight stairs to their second-story apartment was very challenging. It had the potential to be a dangerous situation for both Bill and Barb, as she assisted him up and down the stairs. Erik and Bill returned to the gym to practice on the stairs. Bill was able to discharge to his home with his wife. At first, going from a whole team of caregivers to the two of them at home was a big adjustment.
About a week after discharge, the Hollaces moved to a ground floor apartment that eliminated this high-risk for fall situation. The Hollaces were able to utilize home health physical, occupational, and speech therapy, as well, as he adjusted to being home in his own environment. Barb commented that her training time at RHN with Bill was an invaluable resource for their transition to life at home.
Barb recalled that their first stop after leaving RHN was Wendy’s for a hamburger. For months, when Bill was receiving his nutrition via a stomach feeding tube, he often dreamed of having a hamburger. It may have been the best hamburger Bill has ever eaten.
Currently, Bill is using a front-wheeled walker and a four-wheeled walker, when needed. Working with a home health physical therapist, Bill is increasing his stamina and expanding his territory to longer distance walks outside. Some days, the therapists work with Bill to walk in their home without walker assistance for distances up to 200 feet.

The Hollaces renewed their wedding vows in 2012. Their love and support of each other played an important part in Bill’s recovery.
The Hollaces attend church every Sunday. Wednesdays and Saturdays are their adventure days. At first, those days consisted of only driving around, maybe they got something to eat or drink and sat in the parking lot. Bill and Barb tried to do things that wouldn’t overstimulate him as they gradually reintroduced Bill to the world outside the hospital, where he had spent five and a half months. They set goals about when and where they would go and accomplished them one by one.
Bill acknowledged how very scary this process was. He said, “I wouldn’t wish this on my worst enemy.” Bill served in the United States Marine Corps, and as he described it, that even after his service and everything else, even being fired at by the best, “They did a lot of damage, but they couldn’t do the damage that this little bug did to me.”
Bill expressed his thankfulness, as well, wishing to be able to thank everyone who helped him along the way. He hopes that others will have the same opportunities that he did to help them get better. Barb reaffirmed, “What a great opportunity! There were great people at both facilities that really made this journey just so amazing for us. We felt so supported. What a blessing! We wouldn’t be where we are today, except for all their help.”
Today, the Hollaces look forward to enjoying the spring and summer with more walks outside and time in the park. “Life is precious. We are grateful every day for Bill’s life and his ongoing recovery, “ Barb said with a smile. “The best is yet to come.”
Heart disease can cause complications like heart failure, heart attacks, or strokes. When someone experiences an event like this, long-term acute care hospitals (LTACHs) can help.
LTACHs often have cardiovascular programs designed to help patients with chronic or exacerbated cardiac issues like:
- Heart bypass surgery
- Valve replacements
- Abdominal aortic aneurysms
- Complex wound healing … and more.
Patients are referred to LTACHs after initial treatment at “acute care” hospitals when complex medical conditions prevent them from being transferred to lower levels of care, and/or they have more than one serious condition going on.
For example, a patient with heart failure may also be experiencing respiratory failure and could be put on a ventilator to help with breathing.
Heart failure is serious in itself, but now the situation would be even more critical because there’s not enough oxygen passing from the patient’s lungs into the body’s bloodstream. And, the patient would need special medical assistance in healing and weaning from the ventilator.
This is where an LTACH hospital comes in.
LTACH hospitals have specially trained staff and equipment to care for patients with these medically complex needs. Staff members treat situations like this on a daily basis and know how to tailor and provide specialized care to each patient, allowing optimum results and the best chance at recovery.
About Ernest Health
Northern Idaho Advanced Care Hospital is part of Ernest Health, a network of rehabilitation and long-term acute care hospitals. Ernest Health hospitals see patients who are often recovering from disabilities caused by injuries or illnesses, or from chronic or complex medical conditions.Read More
Quick Reference Links
• Contact Us• Career Opportunities at this Hospital
• Price Transparency
• About Ernest Health